Overview of Research Gaps for Selected Conditions in Women's Health Research at the National Institutes of Health: Proceedings of a Workshop—in Brief (2024)
Chapter: Overview of Research Gaps for Selected Conditions in Women's Health Research at the National Institutes of Health: Proceedings of a Workshop — in Brief

Overview of Research Gaps for Selected Conditions in Women’s Health Research at the National Institutes of Health
Proceedings of a Workshop—in Brief
The National Academies of Sciences, Engineering, and Medicine (the National Academies) convened an ad hoc committee with scientific, ethical, regulatory, and policy expertise to address the persistent gaps that remain in the knowledge of women’s health research across the National Institutes of Health (NIH). It was tasked with analyzing the proportion of NIH funding that supports conditions that are female specific and/or more common in women or affect women differently and to determine the level of funding needed to address gaps in women’s health research. The committee was also tasked with developing recommendations regarding the structure of the NIH and the systems and processes needed to ensure optimal women’s health research. To inform its deliberation process, the Committee on Assessment of NIH Research on Women’s Health held a second public workshop on March 7, 2024.1 The discussions included the science of sex differences, research needs within reproductive and gynecologic health, and research efforts aimed at women’s mental and behavioral health, women’s cancers, and nonmalignant gynecologic conditions. Speakers shared suggestions for how to improve and advance women’s health research at NIH (see Box 1).
The workshop represents only part of the committee’s information gathering process; the topics covered are not meant to be comprehensive or cover all women’s health issues, and the complex interactions among these conditions, across the life course. This Proceedings of a Workshop—in Brief summarizes the presentations and discussions and should not be seen as a consensus of the workshop participants, committee, or National Academies.
SCIENCE OF SEX DIFFERENCES
Margaret McCarthy, University of Maryland School of Medicine, studies sex differences in the brain. She noted boys are typically more likely to be born prematurely, suffer injuries at birth, and be diagnosed with neuropsychiatric or neurological disorders originating in development. Conversely, she continued, women are more likely to experience interpersonal sexual violence, suffer from affective disorders and chronic pain, and be diagnosed with autoimmune disorders. Overall, male-biased disorders are typically diagnosed in childhood and female-biased disorders in adulthood. This profound gender bias compels her research team to understand the origins of risk and resilience to brain disorders, said McCarthy. Brain sexual differentiation occurs during a sensitive period early in development. Her lab focuses on the sensitive period when this cellu-
__________________
1 The first public workshop for this study was held on January 25, 2024. More information can be found here: https://www.nationalacademies.org/event/41691_01-2024_assessment-of-nih-research-on-womens-health-meeting-2-part-3 (accessed June 11, 2024).
![]()
lar process occurs in rat brains, so they can examine the cellular and molecular mechanisms by which androgens influence brain development. Since 2002, McCarthy’s lab has produced studies identifying that prostaglandins, normally part of the body’s immune and inflammatory responses, are found in higher concentrations in certain parts of the male rodent brain. Additionally, microglia, innate immune cells, are more activated in parts of the male brain, and there are more mast cells in male brains during this programming process, she said (McCarthy, 2023). McCarthy and collaborators examined postmortem human brains and found that very specific, critical cell types in the cerebellum were affected by inflammation in very young children (Ament et al., 2023). Connecting her basic science results to more translational findings, McCarthy highlighted a broader impact—being male is a leading biological predictor of the relative risk for developmental neuropsychiatric disorders, while inflammation is a leading environmental predictor of relative risk. Looking specifically at autism spectrum disorder, with 4.5 male diagnoses for every one female, McCarthy said some research has posited that this bias exists because of not just male vulnerability to developmental neuropsychiatric disorders, but also female resilience to them. Last, she noted some critical research gaps: the need for greater understanding of how steroid hormones integrate with the nervous and immune systems, more blue-sky research (i.e., research that aims to increase scientific understanding without considering real-world applications) to understand the basic mechanisms of biologically established sex differences beyond disease cases, and greater focus on girls’ health.
Karen Reue, University of California, Los Angeles, shared her work on sex differences in cardiometabolic disease, first highlighting the profound importance of sex differences to metabolism (see Figure 1).2 These differences, she explained, either reflect or contribute to body fat composition, plasma lipid profiles, susceptibility to myocardial infarction and ischemic stroke, and more. Although it was thought that sex chromosomes are mostly important during early development, she said that newer data suggest that sex chromosomes act in every cell in the body throughout the life course.
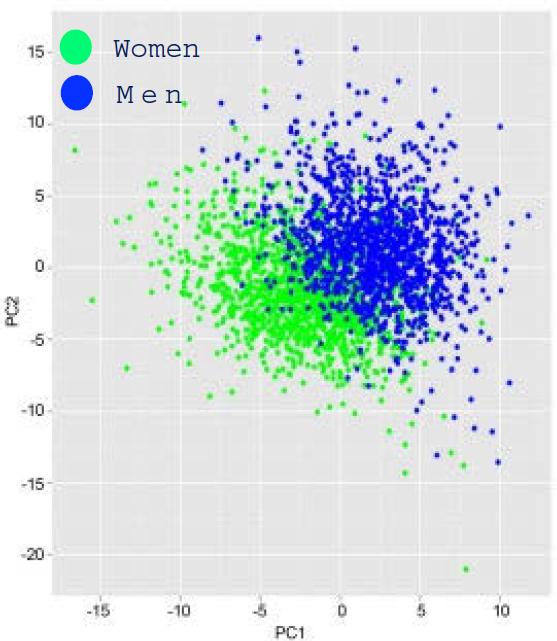
SOURCE: Karen Reue presentation, March 7, 2024; adapted from Mittelstrass et al., 2011; adapted and reprinted under the Creative Commons Attribution 4.0 International CC BY (https://creativecommons.org/licenses/by/4.0/).
Using a four core genotypes (FCG) mouse model that aims to identify the contributions of chromosomal versus gonadal sex, her team determined that chromosomal sex (XX versus XY) influences sex differences in many cardiometabolic traits, including obesity and fatty liver, and adverse effects of drugs, such as statins. They found that specific genes that can escape X chromosome inactivation3 influence these sex differences. Studies with statins in FCG mice revealed that XX chromosomes promote glucose intolerance and reduce beneficial fatty acid levels. These findings translate to humans; similar effects were observed in statin-treated women, suggesting that they may be prevented with specific fatty acid supplementation. Finally, she said that understanding the mechanisms for risk factor prevalence is key because interventions are possible once it is clear why one sex is more susceptible. She added that animal models allow detection of interactions between biological sex and genetic background or environment, while interactions with gender can be studied in humans.
__________________
2 “Metabolites are small molecules (such as amino acids, lipids, peptides, nucleic acids, carbohydrates, vitamins, and minerals) that are intermediate products of biochemical processes that take place in living organisms” (Verma and Gazara, 2021).
3 During early development, one of the X chromosomes in XX cells becomes inactivated, which has the effect of normalizing most of the transcripts on the X chromosome from in an XX and a XY cell. There are some exceptions where genes on the inactivated X are still expressed; these are called “escape” genes.
![]()
WOMEN’S REPRODUCTIVE AND GYNECOLOGIC HEALTH RESEARCH
American College of Obstetricians and Gynecologists
“Women’s health has been underresearched throughout its history,” said Christopher Zahn, American College of Obstetricians and Gynecologists. Not including women in research on topics such as cardiovascular disease (CVD), HIV medications, and COVID-19 vaccination has led to harm. He explained that despite some progress, including the NIH Revitalization Act and reclassification of pregnant women from “vulnerable” to “scientifically complex,” there is still a long way to go. Additional concerns, he added, include the exclusion of pregnant women from trials investigating complex conditions, weighing fetal and maternal risk versus benefit, and addressing ethical considerations of justice, autonomy, and informed consent.
Zahn highlighted research gaps, such as the multifactorial nature of maternal morbidity and mortality. He noted that a contributor to gaps in data is the bundled billing codes and global payment system for obstetrics, and the lack of a uniform definition for severe maternal morbidity is also a challenge to robust data collection. Additional needs he highlighted include research on maternal health, including mental health, environmental impacts on pregnancy and lactation, addressing misinformation, obesity prevention, endometriosis, examining unique risks for women in the military, and reproductive health in the LGBTQ+ community. Last, he emphasized the importance of health equity. Zahn noted that although race and ethnicity are used as variables in research, they are only proxies, and it is necessary to identify real, underlying risk factors to appropriately intervene.
Coalition to Expand Contraceptive Access (CECA)
Jamie Hart, CECA, shared that the organization began working in 2019 to help support the potential change in presidential administration, bringing together evidence and expertise to develop relevant recommendations. CECA sees sexual and reproductive health equity as systems that ensure people have what they need to attain their highest level of sexual and reproductive health, including self-determination and support from government and health care. Given the recent Dobbs v. Jackson Women’s Health Organization ruling, CECA has been convening stakeholders to discuss potential impacts on contraceptive access and needed collective efforts and sharing its process and focus areas (see Figure 2). She highlighted the pivotal role of research in understanding people’s needs and ensuring policy and practice are supported by evidence.
“We need to meaningfully consider how we are engaging communities throughout the research lifecycle and what impact our research is having,” said Hart. Last, she shared the equity-informed principles from the CECA research roadmap which they use to guide contraceptive access strategy development (CECA, 2021):
- Ground contraceptive access research in a holistic vision of sexual and reproductive health that centers justice, equity, autonomy, and choice.
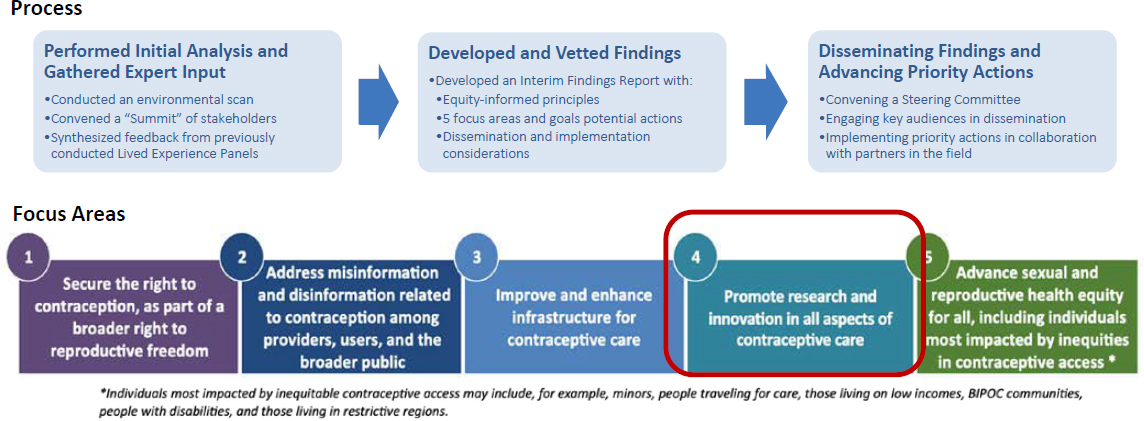
SOURCE: Jamie Hart presentation, March 7, 2024.
![]()
- Interrogate and re-evaluate the research practices that have guided us.
- Honor and embrace communities as equal partners throughout the research process.
- Understand and reflect the impact of the historical, sociocultural, political, and economic contexts that influence the lived experiences of community members.
- Design actionable research that can be used to impact the lives of individuals and communities through changes in systems, policies, and practice.
Society of Family Planning (SFP)
Amanda Dennis, SFP, introduced her organization as an academic society comprising more than 1,700 members across the field of abortion and contraception. Although NIH is a critical source of funding, only 0.3 percent of the NIH’s $331 billion total funding 2009–2018 was invested in family planning research, she said. She explained that SFP believes expansion is needed because abortion and contraception impact people over much of their lifespan. As a passthrough grant maker, she said, SFP partners closely with private philanthropies and individuals to generate essential research funding (awarding more than $75 million in this area). Despite huge new issues for abortion right now, Dennis said, long-standing questions remain unanswered because of the lack of investment. She offered high-level priorities from SFP’s perspective, including documenting changes in abortion access and delivery, understanding short- and long-term ramifications for restrictions, and implications for the workforce. She shared similar priorities for contraception, within the context of ensuring evidence-informed and person-centered care, including technological advances and innovations, and addressing mis- and disinformation. For both abortion and contraception, she called for more research to ensure the ability to provide care for people with specific health care needs and those experiencing systematic oppression and care financing and affordability.
Black Mamas Matter Alliance (BMMA)
BMMA is a national network of Black women–led organizations and multidisciplinary professionals whose work is deeply rooted in reproductive justice, birth justice, and the human rights framework, said Angela Doyinsola Aina, BMMA. She highlighted its mission to center Black mothers, including cis women, transgender individuals, gender non-conforming and/or gender expansive individuals with or without the capacity for pregnancy, and those who care for and mother families and communities, whether they have given birth or not. BMMA aims to shift culture and advance maternal and reproductive health equity domestically and globally. BMMA works to change policy using a human rights framework to address health inequities and improve the health outcomes of Black women and birthing people, advancing care by promoting holistic, respectful, and comprehensive maternal and reproductive health approaches. Aina shared that it has developed research guidelines and a policy agenda to lay the foundation and scope of work for the Black maternal health, rights, and justice movement (BMMA, 2023). Recounting the deeply unethical research conducted on Black individuals throughout history, Aina emphasized the disproportionate impact of the U.S. maternal health crisis on Black mothers and birthing people. Despite this unethical history in research, she emphasized BMMA’s commitment to the power and potential of research to transform lives for the better. She offered policy and research recommendations, highlighting data disaggregation and antiquated clinical categories, investment in and consultation with Black women and birthing people as researchers, and research in historically underfunded reproductive health areas.
Discussion
The majority of the discussion focused on barriers for the inclusion of pregnant women and other subgroups in clinical research, along with potential strategies for NIH. Zahn said that although adequately powering studies for pregnant women is challenging, efforts need to be made to appropriately include them. He noted the misperception that they do not want to participate in research. However, he added that challenges persist in encouraging clinician-scientists in non-OB/GYN specialties to conduct research. To make it more feasible, Dennis suggested NIH could make overt statements embracing both biological and social factors impacting reproductive health, and Zahn proposed requiring the inclusion of pregnant women for grants to increase accountability.
![]()
WOMEN’S MENTAL AND BEHAVIORAL HEALTH RESEARCH
Hormonal Triggers and the Menstrual Cycle
Tory Eisenlohr-Moul, University of Illinois at Chicago College of Medicine, shared her lab’s work on understanding hormonal triggers relevant to mental health. The menstrual cycle can cause significant changes in emotion and behavior in some people, said Eisenlohr-Moul, and certain symptoms tend to cluster in specific phases of the menstrual cycle (see Figure 3). She highlighted premenstrual dysphoric disorder (PMDD), the sole diagnosis related to menstruation and mental health. Due to problems with false-positive reporting, daily symptom ratings across 2 months are required for PMDD diagnosis; however, studies have shown that this level of data collection is not feasible in most clinical settings.
Even with limited data, PMDD is clearly quite prevalent, and premenstrual exacerbation (PME), where chronic mental health symptoms are worsened, is even more prevalent, said Eisenlohr-Moul. These cyclical emotional changes are also linked to suicidality, and the risk of hospitalization for suicide attempts peaks during menses, she added (Eisenlohr-Moul et al., 2022; Saunders and Hawton, 2006). Eisenlohr-Moul pointed out the mounting evidence showing multiple hormonal triggers and sensitivities may contribute to pathophysiology. In closing, she highlighted research gaps, including the need for large-scale studies in patients with substance use disorder, longitudinal cohort studies to better understand the natural course of PMDD/PME, and development of more and higher-precision treatments, whether pharmaceutical or behavioral.
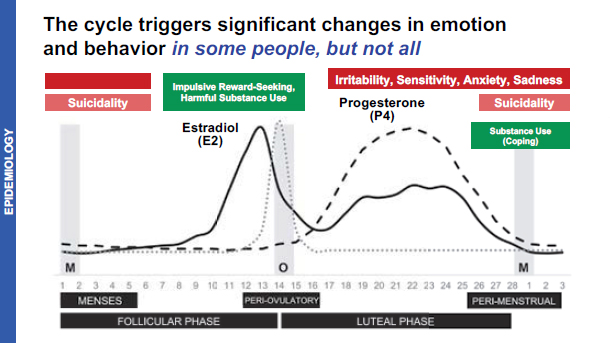
SOURCE: Tory Eisenlohr-Moul presentation, March 7, 2024.
Perinatal Psychiatric Illness
Kristina Deligiannidis, Zucker Hillside Hospital at North-well Health, highlighted the most prevalent perinatal mental health disorders (e.g., depression, anxiety, posttraumatic stress disorder), affecting more than one in five individuals. They are the most common complication in pregnancy and the year following delivery and the leading cause of pregnancy-related death in the United States (Trost et al., 2022). The prevalence of perinatal mood and anxiety disorders and severe mental illness (bipolar and psychotic disorders) doubled 2006–2015 (McKee et al., 2020). She shared the numerous adverse outcomes linked to these disorders, including increased rates of maternal health conditions, preterm labor and birth, increased requirement for cesarean delivery, lactation failure, and impaired child cognitive or emotional and behavioral development. Despite the bidirectional relationships between some of these illnesses, she said, their mechanisms are not understood. She explained that the pathophysiology is also poorly understood, although several potential mechanisms are being investigated, including endocrine, epigenetic, inflammatory, synaptic transmission, neural network, stress, and neurosteroid. Despite robust data on psychotherapies for perinatal patients, she said, no randomized clinical trials of relevant pharmacotherapies exist on which to base clinical recommendations. She emphasized the paucity of such psychiatry clinical treatment studies versus research outside the peripartum period, leading to prescribing in pregnancy and lactation without efficacy or safety data. In closing, she compared the costs of not treating these disorders, estimated at $14.2 billion annually, with the investment in annual federal funding of only $54 million in 2017 (Mind the Gap, 2019).
Considering Childhood Adversity as a Risk Factor During Perimenopause
C. Neill Epperson, University of Colorado School of Medicine, called attention to the importance of considering the lifespan when working to understand and improve women’s health. Most people do not think about adverse childhood experiences (ACEs) and their impact on risk for cognitive and mood concerns during peri- and post-menopause, she said. Yet this is an important period to study, as women can be in perimenopause for a decade or more and experience many symptoms, including depres-
![]()
sion, anxiety, sleep disturbances, vasomotor symptoms, and cognitive complaints. Epperson compared examples of a woman in natural menopause, who may feel a slow progression of symptoms, with another woman who undergoes surgical menopause, which often happens earlier and abruptly changes hormone levels, resulting in rapid symptom onset. However, how surgical menopause impacts the brain is not often raised in these decision-making discussions, she added. Although women are living longer, the age of the final menstrual period has not changed much in the last 100 years, said Epperson, and brains have not evolved to optimally manage up to 40 postmenopausal years.
Childhood Adversity and Brain Health
Stress and trauma can have epigenetic effects, said Epperson, and alter brain structure and function, the microbiome, and response to hormonal changes; however, more research is needed. Females are more likely than males to report four or more ACEs. Research has shown that two or more ACEs before puberty is associated with a 2.6-fold increase in first onset of major depressive illness in perimenopause, she explained (Epperson et al., 2017). Similarly, women in higher-ACE groups also report increased executive functioning difficulties across multiple cognitive domains, including motivation for work, sustained attention and alertness, and working memory, Epperson said. Menopause can also be associated with increased inflammatory markers, which is particularly true for high-ACE women in late perimenopause, she added (Metcalf et al., 2021). Inflammation and ACEs together can also adversely impact verbal memory. Her research has found treating high-ACE women within the first postmenopausal decade with estradiol alters brain response during working memory task performance (Shanmugan et al., 2017), suggesting that it may help the dorsolateral prefrontal cortex, which is important for executive function, work more efficiently. This was not observed in postmenopausal women with one or no ACEs. She called for more research on hormonal and nonhormonal treatments for women so that a range of options can be made available.
The discussion also touched on the participation of racially and ethnically minoritized women in research, with Epperson highlighting their lack of inclusion in studies related to surgical menopause. A couple of presenters noted that relationships between research institutions and some communities of color are strained, which can create barriers to research participation. Additionally, several participants discussed the need for studies of perinatal mental health; the interaction of ACEs with geographic location, neighborhood, and race and ethnicity; and the importance of preclinical models and studies in healthy individuals that better elucidate the mechanisms of typical brain responses to hormonal changes, which can then inform studies on suboptimal or pathological responses.
WOMEN’S CANCER RESEARCH
Breast Cancer
Reshma Jagsi, Emory University School of Medicine, shared two lessons from breast cancer research: 1) Striking improvements in mortality have been observed over past decades that reflect multiple moderate gains from screening and treatment improvements, and 2) focusing on treatment optimization is essential. Although the first lesson leads some to believe that work on breast cancer is complete, this is not true, she argued, and strong federal funding in this area is still needed. Highlighting NIH-funded discoveries across disciplines, she noted the improvements in optimizing surgery to move away from disfigurement, reducing burden of radiation treatment with shorter courses, and personalizing systemic therapy, inspired by the growing appreciation for biological heterogeneity. Despite these gains, gaps remain in translating many of these discoveries into practice, she said. For example, although robust evidence shows some women can safely avoid potentially toxic treatments, that does not always translate into practice, and many women pursue unnecessarily aggressive treatments (Jagsi et al., 2017). This overtreatment has downsides, explained Jagsi, such as worsened quality of life, second malignancies after unnecessary radiation, and other side effects, such as cardiac toxicity, cognitive decline, and financial toxicity. To assist in providing the most optimized treatment pathway, she suggested decision support tools (Hawley et al., 2018) and more focus on addressing disparities across age and racial and ethnic groups (Grabinski and Brawley, 2022), disaggregating data to detect more meaningful differences. Last, she argued for greater focus on individuals with inflammatory or metastatic breast cancer,
![]()
prevention and targeting known risk factors, and maintaining and growing a thriving workforce within women’s health research (Beeler et al., 2019).
Gynecologic Cancer
Ovarian cancer is much less common than breast cancer, said Beth Y. Karlan, University of California, Los Angeles Jonsson Comprehensive Cancer Center, but more than 12,700 women will die from it in 2024. It continues to be a high-mortality cancer, with the death-to-incidence ratio more than three times that of breast cancer. The overall 5-year survival rate remains around 50 percent, much of which is due to the late stage of presentation and lack of reliable screening, she explained. However, the incidence has declined in recent years, likely related to the increased use of birth control pills, which can reduce risk by about 50 percent when used for 10+ years. Recent decreases in mortality are likely due to the discovery and availability of better chemotherapy and targeted treatment agents. Karlan shared takeaways from a 2016 National Academies report, noting that ovarian cancer is not one disease, and failure to look at cell type–specific research has hampered advancements, as each type should be studied separately to better embrace precision oncology. Additionally, most ovarian cancers begin in the fallopian tube, not the ovary. She also called attention to racial disparities in outcomes and called for improved access to guideline-concordant care and wider dissemination of information on standards of care and clinical trials to address these disparities. A quarter of ovarian cancers are associated with an inherited predisposition. Although universal genetic testing for women with ovarian cancer has been recommended since 2010, only about one-third are tested, she noted. Fully implementing this guideline could open opportunities for primary prevention and targeted therapies. Karlan said more translational research and clinical trials are needed, yet funding-to-lethality scores show an 18-fold difference in funding relative to breast cancer, limiting innovation.
Victoria L. Bae-Jump, University of North Carolina at Chapel Hill School of Medicine, centered her remarks on obesity-driven endometrial cancer and remaining challenges to improve outcomes. As the fourth most common cancer among women in the United States, endometrial cancer is the only major type increasing in frequency and mortality. It is split into two categories; Type 1 is more common and has higher 5-year survival rates, and Type 2 is often much more aggressive, has lower survival rates, and is more common in Black patients. Obesity, diabetes, and insulin resistance are risk factors for both types. She shared her thoughts on why outcomes are worsening, including limited public awareness, lack of funding and treatment options, the persistent obesity epidemic, the rise in more aggressive subtypes, and worsening disparities for Black women. Bae-Jump said many researchers have sought to find the best interventions to break the strong link with obesity, using mouse models to test how metabolic and inflammatory pathways, immune cells, and the microbiome could be affected. Four key interventions she has focused on are intermittent fasting, exercise (high-intensity interval training), bariatric surgery, and, most recently, weight loss drugs. But many challenges remain, said Bae-Jump, with the largest being the lack of prospective population-based epidemiological studies that include social and biological factors for understanding worsening outcomes, rising disparities for Black women, and the relationship of both to the obesity epidemic.
RESEARCH ON NONMALIGNANT GYNECOLOGIC CONDITIONS
Uterine Fibroids
Erica Marsh, University of Michigan Medical School, explained fibroids as noncancerous masses with clear walls that can vary from microscopic to over 30 centimeters in diameter. They are the leading cause of hysterectomy in the United States, she said, accounting for more than endometrial, ovarian, or cervical cancer. But, she noted, fibroids receive just $17 million in NIH funding annually. Between 30 and 50 percent of women with fibroids have clinical symptoms, but it often takes years from the onset of symptoms to receive a diagnosis. Common symptoms include heavy menstrual bleeding—often causing anemia—pelvic pressure, low back pain, infertility, and constipation. Although millions are affected by this condition, said Marsh, treatments are quite limited, including some medical, radiological, and surgical (removing the fibroids or the entire uterus) treatments. Risk factors include race, obesity, hypertension, pelvic infections, alcohol, and older age. Race is one of the most significant, and that differential can start before most individuals know they have fibroids (Marsh et al., 2013).
![]()
Black women have more, earlier, and larger fibroids, said Marsh, but outcome disparities also exist (e.g., being offered treatment, patient experiences, and uterine-sparing treatment). To answer remaining research questions, she called for more funding for the entire disease trajectory, such as pathophysiology, development of in vitro models, expansion of analyses to include diverse groups, and more effort to develop nonhormonal therapies. She concluded by noting that beyond the many questions that need to be answered within clinical and basic science research, areas within health services and health behavior research also need to be explored to ensure women understand abnormal symptoms and providers can deliver patient-centered care.
Endometriosis
Steven L. Young, Duke University School of Medicine, explained endometriosis as a chronic persistence of endometrial cells outside the uterine cavity, resulting in inflammation and scarring, and, like fibroids, highly variable symptoms. Patients have an increased risk of pregnancy complications, CVD, autoimmune disease, and some types of ovarian cancer, yet its cause and risk factors remain obscure, he noted. Although it is common, he noted, there has been little progress on understanding pathophysiology in the last 30 years, with no cure and frequent recurrences even after surgery. Barriers such as political and regulatory issues, and the lack of a nonsurgical diagnosis method, prevent professionals from being able to readily diagnose and prevent, treat, or cure endometriosis, said Young. Lacking a diagnostic test limits human research, and testing new treatments is limited because it is often unclear whether pain symptoms are progressive or part of the natural disease history. Additionally, although animal models can be useful for some research aspects, only certain species menstruate and develop endometriosis, and it is quite difficult to monitor for development similar to humans. In closing, he called for an NIH institute focused on women’s health and a return of the NIH-funded Reproductive Medicine Network.
Pelvic Floor Disorders
Carolyn Swenson, University of Utah School of Medicine, shared her primary interest as identifying the underlying mechanisms of disease of pelvic organ prolapse. Pelvic floor disorders comprise a group of common conditions that decrease quality of life, affecting more than 25 million each year. In prolapse, one of the most severe disorders, the pelvic organs descend into and outside of the vaginal opening, she said, which affects up to half of women to some degree. Although up to one in five women have surgery for this condition, she said, there is a high failure rate. Currently, most research funding goes toward incremental improvements in late interventions—the equivalent to waiting until a patient has a heart attack to check her blood pressure, she explained. Until disease mechanisms are understood with effective ways of monitoring progression, treatments cannot be optimized, Swenson stated. To overcome the knowledge gaps and barriers such as strong competing interests and lack of funding, she suggested expanding mentorship opportunities, formalizing research training, creating a dedicated study section at NIH, and expanding the NIH reviewer pool to include experts in women’s health topics.
PARTICPANT PERSPECTIVES
Interested groups and individuals shared their perspectives and priorities during the meeting. Many participants in this session discussed how women’s health is undervalued compared to other areas in medicine and the gap in women’s health research—especially in understanding mechanisms that contribute to health and disease across the life course. Several participants noted the limited funding available for women’s health research and individuals voiced the critical need to focus on aspects beyond reproductive years, integrating personal experiences, mental health, and the systemic structures that impact women’s health outcomes. Several participants noted that the funding for certain conditions does not match their prevalence and the vast number of women suffering from them (e.g., polycystic ovary syndrome [PCOS], pelvic floor disorders, genito-pelvic pain disorders, uterine fibroids, and menopause). Last, a few participants called for including patients with lived experience and addressing historical biases and educational gaps in health care to transform women’s health research and care delivery. Several speakers called for investment in more areas of women’s health research, innovation, a life-course approach, and a whole-person approach to research and care.
![]()
Investing in Women’s Health Research
Sasha Ottey, PCOS Challenge, shared her story as a woman with PCOS, fibroids, and a traumatic postpartum period. PCOS is one of the most common hormone disorders, she said, but varies in manifestation, highlighting the complexity of women’s health. Although it affects up to 13 percent of women, Ottey said, PCOS was not included in NIH’s Research, Condition, and Disease Categorization until 2022, after PCOS Challenge’s advocacy work. The funding is now just $9–10 million annually, she noted. Ottey called for commitment to long-term studies; a research approach that explores the condition’s broader spectrum—including metabolic and mental health, and quality-of-life impact; FDA-approved treatments; and equitable funding and focus across diseases.
The lived experience of women with uterine fibroids is a societally dismissed experience in communities worldwide, steeped in millennia-old expectations that women endure immense pain, said Sateria Venable, Fibroid Foundation. Even with extremely heavy bleeding, causing anemia, she recounted the countless times she had to work and care for others despite the pain and symptoms. Research funding should match the population affected, she continued, noting that 70–80 percent of all women will have fibroids by age 50. To improve outcomes and advance this field, she called for more grant opportunities for nonmedical professionals to conduct research and more alternatives to hysterectomies to improve quality of life.
Sarah Cigna, George Washington University, highlighted the lack of funding for research related to vulvar and genito-pelvic pain disorders. She described disparities in the number of research articles between men and women across similar topics (i.e., penile vs. vulvar pain). Without high-quality research, she said, FDA approval cannot be obtained, meaning there is no insurance coverage for treatments, resulting in most patients being unable to access needed care. She added that sexual medicine specialists cannot afford to practice within the insurance model because of reimbursement rates. She requested the committee strongly consider prioritizing sexual health and genital pelvic pain disorders for women because they have been understudied compared to men’s.
Sue Goldstein, San Diego Sexual Medicine, echoed the challenge of underinvestment in women’s health but noted that some areas have been left out completely, such as sexual health. Approximately 40 percent of women experience sexual health issues, including with desire, arousal, orgasm, and pain/genito-pelvic dysesthesia, she said, which is more than men, but funding has been low. Practitioners and the general public continue to be fearful of hormones, and systemic and vaginal estradiol are often grouped together for box warnings on medications despite evidence that they are distinct. She called for more research and understanding, including better treatment options, such as testosterone for women and medications for premenopausal women.
Kim Pettman, patient advocate and former librarian, said that a lot of medical information is in paid databases most people cannot access; many, including doctors and nurses, only use an Internet search. Pettman recommended grants for librarians to teach people to access this information. Pettman also advocated for including the public in every step of the committee’s process, especially people with disabilities and rare and underdiag-nosed conditions. People with this experience must be included if you want things done right, she said.
Michal Elovitz, M.D., Icahn School of Medicine at Mount Sinai, noted the gaps in women’s health research, drawing on her personal health experiences and professional frustration with stagnation in evidence-based care for women across the lifespan. She emphasized the need to invest in fundamental biological research, reiterating the underfunding of women’s health and lack of OB/GYNs involved in decision making at NIH. She advocated for creating new NIH structures to fund multidisciplinary teams, dedicated funding and structures to support women’s health research, and additional funding to increase the women’s health research workforce.
Katie Schubert, SWHR, highlighted the intersectionality of women’s health equity and said better accountability, training, and coordination across NIH Institutes and centers could help resolve some of these issues and improve funding challenges. Regarding the sex as a biological variable (SABV) policy, improving implementation and accountability would greatly benefit women’s health, she noted, including better training researchers to under-
![]()
stand sex differences and ensuring these are considered in research and publishing.
Innovation in Biotechnology
Sheila Mikhail, Biotechnology Innovation Organization’s Women’s Health Initiative Task Force, introduced herself as a poster child for women’s health. She had endometriosis as a young woman. As a lupus patient, she was told that her symptoms were all in her head. Her bilateral breast cancer went undetected over years of mammograms at a top medical center. The task force she represents calls for robust investment in foundational women’s health research. Innovation in biotech is built on the discovery medicine, she said, and it is critical to advance understanding of women’s health to enable more preventive measures and treatments. She argued that foundational research should consider the effects of sex and gender on health.
Onyinye Balogun, of Mission-Driven Tech, discussed its goal to apply modern technology to improve gynecologic cancer care. Despite a decline in overall cervical cancer in the United States, she said, the 5-year survival rate has remained stagnant, and more women are presenting with advanced stages. Focusing on treatments, she explained the painful procedures required to deliver internal radiation to women and saw opportunity for improvement. Eve McDavid, also of Mission-Driven Tech, continued, saying that cervical cancer is the only cancer that is preventable, treatable, and curable. She explained that every $1 spent on preventing a death from cervical cancer returns $26 to the global economy, so more funding is needed (WHO, 2020).
Women’s Health Across the Life Course
Claire Gill, National Menopause Foundation, said studying menopause could have a huge impact, given the connections to osteoporosis, cancer, brain health, heart disease, obesity, mental health, and other conditions. How and why menopause has such an impact on these chronic disease areas is not yet understood, she noted, but research needs to be prioritized to not only address symptoms but also improve outcomes. She urged the committee to prioritize midlife health and women’s menopausal journey.
Monica Laronda, Endocrine Society, echoed comments that although reproductive years are critical components of women’s health, advancing health and gender equity requires including girls and women of all ages. She supported NIH’s SABV policy but noted it needs to be implemented as intended, and NIH should require disaggregated analyses of research participants by biological sex and gonadal hormones. She also emphasized the importance of diversity and inclusion across the biomedical research enterprise and suggested expanding relevant programs to encourage women’s health research. Finally, she emphasized the need to include women’s health research across all institutes and centers.
Miriam Graham, Restore Motion, also advocated for more research across women’s lifespans. She discussed hormone fluctuations, how they affect various health aspects, and the confusion surrounding hormone replacement therapies. Graham called for treating the whole person, specifically highlighting the lack of research-based evidence on exercise to most effectively treat pelvic floor dysfunction. She also pointed out the lack of research on how cyclic hormone levels affect vulnerability to injury and the need for collaboration between researchers and clinicians to improve health and quality of life.
WHOLE-PERSON APPROACH TO RESEARCH
Rachel Rubin, Georgetown University, discussed disparities in medical care and understanding between male and female sexual health. She highlighted the absence of female anatomy in medical education and the need for research, education, and advocacy to improve women’s health care. Rubin called attention to practicing challenges; she had to create her private practice because her patients needed visits longer than 10 minutes. Last, she highlighted the necessity of comprehensive education on all aspects of sexual health, underscoring the need for systemic changes to equip future providers to address women’s sexual health adequately.
Emotional, social, and cultural factors often hold more influence over health outcomes than any isolated data point, said Monica Mo, WellSeek and the SeekHer Foundation. Women are twice as likely as men to experience mental health struggles, because of the systems and structures that dictate power dynamics and continue to disadvantage women. She emphasized the need for a comprehensive approach to help women internally
![]()
address these stigmas while also dismantling the systems that perpetuate them. A SeekHer report found that 83 percent of women report minimizing their needs to avoid burdening others (SeekHer Foundation, 2024) and advocates for an integrated approach that promotes both personal and systems accountability. She called for increased research funding to address root causes of mental health disparities and building culturally relevant, equitable systems to spark connection and tackle isolation.
BOX 1
Suggestions from Individual Speakers and Participantsa
Administrative, Fiscal, and Operational Improvements
- Utilize intersectional approaches to data disaggregation and include priority populations in such decisions. (Aina, Jagsi)
- Invest in more “blue-sky” research to understand the basic mechanisms of biological sex differences in risk factors, disease prevalence, pathology, and progression. (McCarthy, Reue)
- Prioritize studies on normal physiological processes in women, separately from the study of specific psychiatric illnesses. (Deligiannidis, Eisenlohr-Moul)
- Prioritize funding mechanisms that include human and animal research to enhance bidirectional translation of findings that will lead to (1) a mechanistic understanding of adaptive and maladaptive brain responses to stress and ovarian hormone changes across the lifespan and (2) identification of interventions that target mechanisms for psychopathology and suboptimal brain aging. (Epperson)
- Empower Black-led and -centered community-based organizations with funding and means to execute their own solutions; develop health equity impact tools to assess consequences of community initiatives. (Aina)
Enhancing Research and Understanding
- Conduct clinical trials that include Black women and birthing people of all sexual orientations, gender identities and expressions, sizes, abilities, colors, nationalities, ethnicities, languages, immigration statuses, marital statuses, religions, housing statuses, occupations, and ages. (Aina)
- Develop exclusive clinical trials for perinatal patients to address pregnancy-specific mental health disorders. (Deligiannidis)
- Expand mentorship opportunities and formalized research training for pelvic floor disorders and for clinician scientists in obstetrics and gynecology overall. (Swenson)
Research Gaps and Priority Areas
- Explore how Dobbs v. Jackson Women’s Health Organization affected the relevant workforce as well as access to, use of, quality of, and provision of contraception. (Hart)
- Focus on medical and psychiatric maternal morbidity and mortality (Deligiannidis, Zahn), young girls’ health (McCarthy), contraception and abortion access and delivery (Dennis, Hart), and menopause (Epperson) in research.
- Investigate the underlying structural and social drivers of racial and ethnic disparities in outcomes. (Bae-Jump, Marsh, Zahn)
continued
![]()
BOX 1 Continued
- Ensure patients are receiving care that follows national guidelines for ovarian cancer to increase survival rates. (Karlan)
- Undertake longitudinal cohort studies to better understand premenstrual dysphoric disorder and premenstrual exacerbation of existing mental health conditions. (Eisenlohr-Moul)
- Improve understanding of steroid hormones and how they integrate with the nervous and immune systems. (McCarthy)
- Improve understanding of sex chromosome influence on lifetime sex differences in health and disease. (Reue)
- Improve understanding of the lifetime effects of stress and trauma on the function and structure of the brain, microbiome, and hormonal response. (Deligiannidis, Epperson)
- Undertake prospective population-based epidemiological studies of histological and molecular subtypes of endometrial cancer and their intersection with race, obesity, and social determinants of health. (Bae-Jump)
a This list is the rapporteur’s summary of points made by the individual speakers identified, and the statements have not been endorsed or verified by the National Academies of Sciences, Engineering, and Medicine. They are not intended to reflect a consensus among workshop participants.
REFERENCES
Ament, S. A., M. Cortes-Gutierrez, B. R. Herb, E. Mocci, C. Colantuoni, and M. M. McCarthy. 2023. A single-cell genomic atlas for maturation of the human cerebellum during early childhood. Science Translational Medicine 15(721):eade1283.
Beeler, W. H., L. M. Cortina, and R. Jagsi. 2019. Diving beneath the surface: Addressing gender inequities among clinical investigators. The Journal of Clinical Investigation 129(9):3468–3471.
BMMA (Black Mamas Matter Alliance). 2023. Black mamas matter: In policy and practice. A policy agenda for the black maternal health, rights, and justice movement. Atlanta, GA: Black Mamas Matter Alliance.
CECA (Coalition to Expand Contraceptive Access). 2021. Priority roadmap for policy-ready contraceptive research. Sacramento, CA: Coalition to Expand Contraceptive Access.
Eisenlohr-Moul, T., M. Divine, K. Schmalenberger, L. Murphy, B. Buchert, M. Wagner-Schuman, A. Kania, S. Raja, A. B. Miller, J. Barone, and J. Ross. 2022. Prevalence of lifetime self-injurious thoughts and behaviors in a global sample of 599 patients reporting prospectively confirmed diagnosis with premenstrual dysphoric disorder. BMC Psychiatry 22(1):199.
Epperson, C. N., M. D. Sammel, T. L. Bale, D. R. Kim, S. Conlin, S. Scalice, K. Freeman, and E. W. Freeman. 2017. Adverse childhood experiences and risk for first-episode major depression during the menopause transition. Journal of Clinical Psychiatry 78(3):e298–e307.
Grabinski, V. F., and O. W. Brawley. 2022. Disparities in breast cancer. Obstetrics and Gynecology Clinics of North America 49(1):149–165.
Hawley, S. T., Y. Li, L. C. An, K. Resnicow, N. K. Janz, M. S. Sabel, K. C. Ward, A. Fagerlin, M. Morrow, R. Jagsi, T. P. Hofer, and S. J. Katz. 2018. Improving breast cancer surgical treatment decision making: The iCanDecide randomized clinical trial. Journal of Clinical Oncology 36(7):659–666.
Jagsi, R., S. T. Hawley, K. A. Griffith, N. K. Janz, A. W. Kurian, K. C. Ward, A. S. Hamilton, M. Morrow, and S. J. Katz. 2017. Contralateral prophylactic
![]()
mastectomy decisions in a population-based sample of patients with early-stage breast cancer. JAMA Surgery 152(3):274–282.
Marsh, E. E., G. E. Ekpo, E. R. Cardozo, M. Brocks, T. Dune, and L. S. Cohen. 2013. Racial differences in fibroid prevalence and ultrasound findings in asymptomatic young women (18–30 years old): A pilot study. Fertility and Sterility 99(7):1951–1957.
McCarthy, M. M. 2023. Neural control of sexually dimorphic social behavior: Connecting development to adulthood. Annual Review of Neuroscience 46:321–339.
McKee, K., L. K. Admon, T. N. A. Winkelman, M. Muzik, S. Hall, V. K. Dalton, and K. Zivin. 2020. Perinatal mood and anxiety disorders, serious mental illness, and delivery-related health outcomes, United States, 2006–2015. BMC Womens Health 20(1):150.
Metcalf, C. A., R. L. Johnson, E. W. Freeman, M. D. Sammel, and C. N. Epperson. 2021. Influences of the menopause transition and adverse childhood experiences on peripheral basal inflammatory markers. Brain, Behavior, & Immunity—Health 15:100280.
Mind the Gap. 2019. Mind the gap: A strategic roadmap to address America’s silent health crisis: Untreated and unaddressed perinatal mental health disorders. Portland, OR: Postpartum Support International.
Mittelstrass, K., J. S. Ried, Z. Yu, J. Krumsiek, C. Gieger, C. Prehn, W. Roemisch-Margl, A. Polonikov, A. Peters, F. J. Theis, T. Meitinger, F. Kronenberg, S. Weidinger, H. E. Wichmann, K. Suhre, R. WangSattler, J. Adamski, and T. Illig. 2011. Discovery of sexual dimorphisms in metabolic and genetic biomarkers. PLOS Genetics 7(8):e1002215.
NASEM (National Academies of Sciences, Engineering, and Medicine). 2016. Ovarian cancers: Evolving paradigms in research and care. Washington, DC: The National Academies Press.
Saunders, K. E., and K. Hawton. 2006. Suicidal behaviour and the menstrual cycle. Psychological Medicine 36(7):901–912.
SeekHer Foundation. 2024. SeekHer Shift: 2024 Report on Achieving Wellness & Equity in Women’s Mental Health. San Diego, California: WellSeek.
Shanmugan, S., J. Loughead, W. Cao, M. D. Sammel, T. D. Satterthwaite, K. Ruparel, R. C. Gur, and C. N. Epperson. 2017. Impact of tryptophan depletion on executive system function during menopause is moderated by childhood adversity. Neuropsychopharmacology 42(12):2398–2406.
Trost, S. L., J. Beauregard, G. Chandra, F. Njie, J. Berry, A. Harvey, and D. A. Goodman. 2022. Pregnancy-related deaths: Data from maternal mortality review committees in 36 US states, 2017–2019. Atlanta, GA: Centers for Disease Control and Prevention.
Verma, S., and R. K. Gazara. 2021. Next-generation sequencing: An expedition from workstation to clinical applications. In Advances in ubiquitous sensing applications for healthcare, translational bioinformations in healthcare and medicine Vol. 13, edited by K. Raza and N. Dey. Pp. 29-47.
WHO (World Health Organization). 2020. A cervical cancer-free future: First-ever global commitment to eliminate a cancer. https://www.who.int/news/item/17-11-2020-a-cervical-cancer-free-future-first-ever-global-commitment-to-eliminate-a-cancer (accessed June 3, 2024).
![]()
DISCLAIMER This Proceedings of a Workshop—in Brief has been prepared by Megan Snair as a factual summary of what occurred at the meeting. The statements made are those of the rapporteur or individual workshop participants and do not necessarily represent the views of all workshop participants; the planning committee; or the National Academies of Sciences, Engineering, and Medicine.
*The National Academies of Sciences, Engineering, and Medicine’s consensus study committee on the Assessment of NIH Research on Women’s Health is solely responsible for organizing this workshop, identifying topics, and choosing speakers. The responsibility for the published Proceedings of a Workshop—in Brief rests with the institution.
MEMBERS OF THE COMMITTEE ON THE ASSESSMENT OF NIH RESEARCH ON WOMEN’S HEALTH Sheila P. Burke (Cochair), Harvard University, Baker Donelson; Alina Salganicoff (Cochair), KFF; Neelum T. Aggarwal, Rush University; Veronica Barcelona, Columbia University School of Nursing; Alyssa M. Bilinski, Brown University; Chloe E. Bird, Tufts Medical Center; Susan Cheng, Cedars-Sinai Medical Center; Felina Cordova-Marks, University of Arizona; Sherita H. Golden, Johns Hopkins Medicine, Holly A. Ingraham, University of California—San Francisco; Robert M. Kaplan, Stanford University; Nancy E. Lane, University of California—Davis Health System; Jane E. Salmon, Hospital for Special Surgery; Cornell University; Crystal Schiller, UNC School of Medicine; Angeles Alvarez Secord, Duke University Health System; Methodius G. Tuuli, Brown University, Women & Infants Hospital; Bianca D.M. Wilson, University of California, Los Angeles.
REVIEWERS To ensure that it meets institutional standards for quality and objectivity, this Proceedings of a Workshop—in Brief was reviewed by Michelle Debbink, University of Utah; Jane E. Salmon, Weill Cornell Medical College of Cornell University; and Michael Liebman, IPQ Analytics, LLC. Leslie Sim, National Academies of Sciences, Engineering, and Medicine served as the review coordinator.
SPONSORS This Project has been funded in whole with Federal funds from the Office of Research on Women’s Health, National Institutes of Health, Department of Health and Human Services, under Contract No. HHSN263201800029I, Task Order No. 75N98023F00005.
STAFF Amy Geller, Study Director; Aimee Mead, Program Officer; Luz Brielle Dojer, Research Associate; Maggie Anderson, Research Assistant; Rachel Riley, Senior Program Assistant.
For additional information regarding the workshop, visit https://www.nationalacademies.org/event/41979_03-2024_assessment-of-nih-research-on-womens-health-meeting-3.
Suggested citation: National Academies of Sciences, Engineering, and Medicine. 2024. Overview of research gaps for selected conditions in women’s health research at the National Institutes of Health: Proceedings of a workshop—in brief. Washington, DC: The National Academies Press. https://doi.org/10.17226/27932.